

Transepithelial or transmucosal abutments may be key to maintaining peri-implant health.
Introduction
When restoring a dental implant, there is always a transmucosal component that needs effective sealing to protect it from the oral environment. This union, which is created during osseointegration of the implant, is functionally similar to natural teeth, but biologically different.
According to the literature, the greatest peri-implant bone loss usually occurs during the first six months after the prosthetic loading of the implants. This confirms that it happens after the biological space is invaded, destabilizing the tissues and bone resorption.
Due to this peri-implant bone loss, the treated surface of the implant may be exposed to the oral medium and cause some type of inflammatory pathology. These diseases are currently the most commonly studied subjects in implantology.
Although the prevalence of peri-implant diseases owes to many factors, there are some risk indicators associated with its appearance, including the restoration design and its implant-prosthesis interface.
Transepithelial or transmucosal abutments may be key to maintaining peri-implant health. Their main function is to distance the crown-abutment micro-gap from the bone margin while the biological width is re-established apically, allowing for an optimal mucosal seal.

These attachments allow for the creation of a screwed prosthesis with a correct passive fit in immediate loading treatments. Moreover, they minimize handling of the tissues during the creation of the final prosthesis, improving the therapeutic results and preventing complications later on.
Clinical case
A patient with bruxism, with no relevant pathological precedents, came to the clinic with a worn and ill-fitting removable partial denture with a loss of vertical dimension and mobility of anteroinferior pieces.
The upper jaw presented an overdenture retained by a bar screwed into three implants with a loss of anatomy in the acrylic teeth. He mentioned a constant loosening of the screws and discomfort as a result.
Treatment plan
Multiple extractions and post-extraction implants with immediate loading were planned.
We decided to restore the upper arch with a new overdenture and look for a fixed prosthetic solution in the lower arch. The aim was to achieve good stability in the restorations, return the lost vertical dimension and find an acceptable esthetic.
Surgery
With the patient’s consent, we conducted the implant placement surgery on the jaw after asepsis and antisepsis of the operative field and under local anesthesia (articaine HCL and epinephrine 1:100.000).
We surgically removed the anteroinferior pieces and carefully fixed and curetted the alveolar beds in order to place the implants in the same operation.
We placed five AVINENT OCEAN CC implants in positions 34 (4 x 11.5 mm), 32, 42, 44 (3.5 x 13 mm) and 46 (4 x 10 mm). We chose implants with a conical connection to achieve a good biomechanical union and guarantee the prosthetic stability of the restoration.
We achieved a very good primary stability (initial torque of 30 Ncm or higher) in all the implants, so we decided to perform immediate temporization.
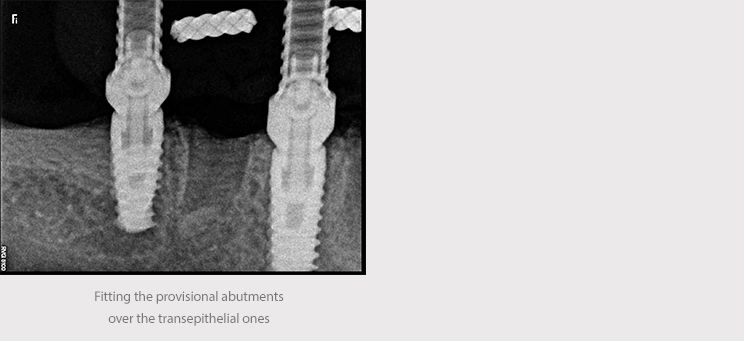
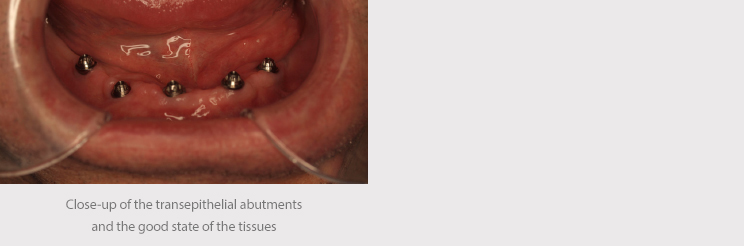
We placed straight transepithelial abutments in different sizes in order to achieve a change of platform and allow the correction of height imbalances in the post-extraction implants. The surgical wound was cleaned with physiological saline and sutured with mattress stitching using 4 mm nylon.

An impression of the implants was taken using an open cup technique, with AVINENT caps and polyether material (Impregum, 3M). This was sent to the laboratory along with a record of occlusion and impression of the antagonist.
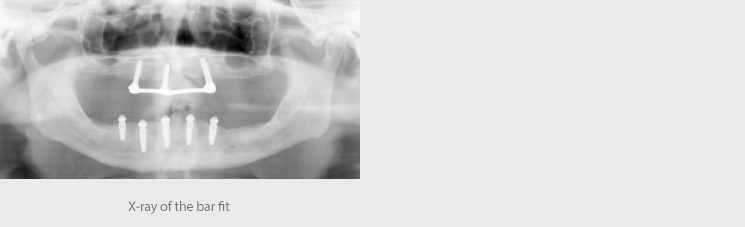
We received the acrylic denture on transepithelial abutments 24 hours later and it was placed in the mouth under local anesthesia. The provisional prosthesis was screwed to 25 Ncm of torque, reviewing the proper fit of the abutments via X-ray. The occlusion was adjusted and polished.
After the instructions for proper maintenance and hygiene of the prosthesis, the patient was referred for a general check-up and the removal of the suture one week later.
Final prosthesis
Three months after the implants were placed, we repeated the operation to take an impression to create the final prosthesis.
One of the advantages of these transmucosal elements is the fact that they make it easier to take impressions, moving them to the paragingival level, and thereby prevent excessive handling of the tissues during preparation of the final prosthesis.
The impression of the lower jaw was performed digitally, with the Trios intraoral scanner (3Shape).
The impression of the upper jaw was performed with a conventional trailing technique and polyether material (Impregum, 3M).
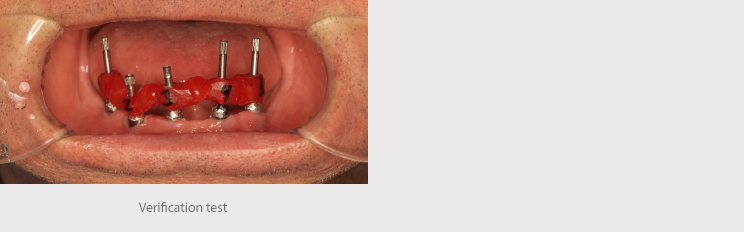
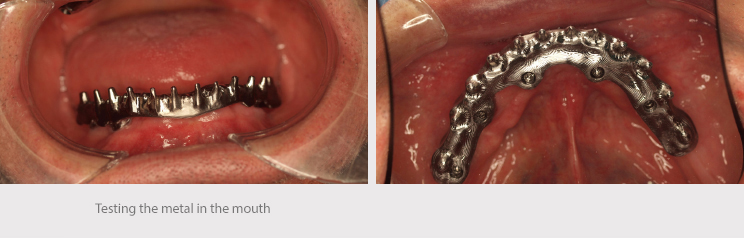
We conducted a test to verify the position of the implants and tested the teeth to assess occlusion, the vertical dimension and esthetic and phonetic aspects.
The Corus Garbident laboratory in Vitoria designed both structures that were milled at CORE3DCENTRES.
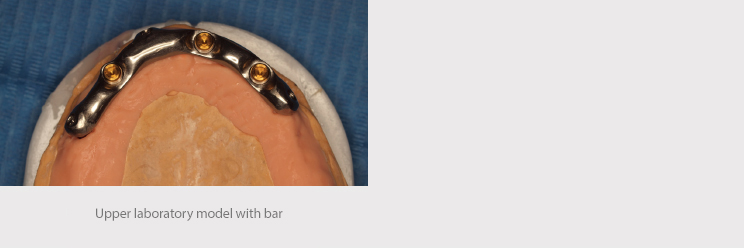
In the upper jaw, a micro-milled bar screwed to three implants was screwed to 30 Ncm, with anchorages for the overdenture (Locator).


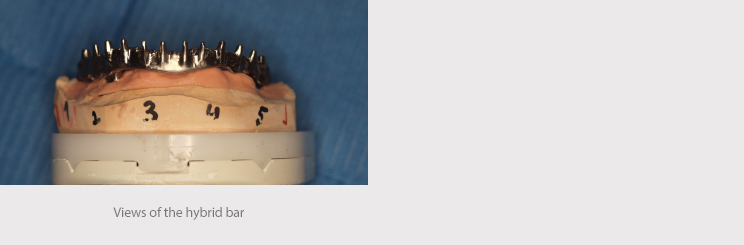
The lower structure was a hybrid bar on milled transepithelial abutments screwed to 20 Ncm.


The occlusion was adjusted and impressions were taken to produce a rigid acrylic night guard to control the patient’s parafunctional habits.

Case conclusion
Healthy tissue around the implant is key to the overall success of the treatment: health, function and esthetics.
To achieve this, a good prosthetic restoration design may be one of the most important factors, ensuring an optimal seal in the peri-implant connective tissue, protecting the implant from the external environment and thereby preventing remodeling of the bone.
In this case, the goals set out in the planning stage were achieved: function, esthetics and a better life for the patient by providing him with high-quality restorations.